US Charges 91 in $295 Million Health Care Fraud Scheme
Authorities have cracked down on Medicare fraud involving nearly $300 million in false billings, the largest amount since 2009, the U.S. Department of Justice announced Wednesday.
As a result of the $295 million fraud 91 people were charged including doctors, nurses, health care company owners and executives in six different cities, the Department said.
Charges include conspiracy to defraud the Medicare program, violations of anti-kickback statutes, and money laundering.
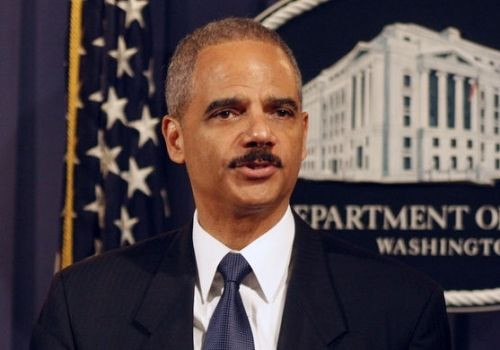
"The charges are based on a variety of alleged fraud schemes involving various treatments and services that were not medically necessary – and, oftentimes, were never even provided," Attorney General Eric Holder said in a press conference today.
Holder emphasized that this is the highest amount of false billings targeted in a single takedown since the launch of the Health Care Fraud Prevention and Enforcement Action Team – known as HEAT – in 2009.
Published by Medicaldaily.com



























