Veterans With PTSD Show Unusual Activity In Brain Regions Unrelated To A Natural Fear Response
Unusual activity occurred in several brain regions, a new study showed, whenever combat veterans with post-traumatic stress disorder looked at images only vaguely similar to an original trauma. This suggests PTSD treatment strategies could be improved by focusing on tangential triggers and not just the trauma itself, say the Duke Medicine and Durham VA Medical Center researchers.
“People with posttraumatic stress disorder grow anxious based on reminders of past trauma and generalize that fear to a variety of triggers that resemble the initial trauma,” Dr. Rajendra A. Morey, an associate professor at Duke and director of the Neuroimaging Lab at the Durham VA Medical Center, stated in a press release.
Over time, symptoms proliferate as a result of patients generalizing their fears to a variety of new triggers, Morey explained. By creating an accurate map of this process, he and his co-researchers hope to identify the specific brain regions involved in behavior changes among PTSD patients.
Mapping Circuits, Mapping Fear
For the study, the research team enrolled 67 military veterans who had been deployed to conflict zones in Iraq or Afghanistan after Sept. 11, 2001, and who had been involved in traumatic events. Of these soldiers, 32 were diagnosed with PTSD and 35 were not. To begin, both groups underwent MRI while being shown a series of five images, depicting faces expressing a range of emotions from neutral to frightened. The scans of both groups showed similar activation patterns.
Next, the researchers replayed these images for both groups outside the brain scanner. However, this time when viewing the middle image — the face showing moderate fear — the participants received a mild electric shock. Then, the patients underwent another MRI scan as they viewed the five faces once again.
What happened here? Among the non-PTSD participants, brain activity increased when they saw the middle face (the one image associated with the mild shock). However, the PTSD patients showed increased brain activity when they saw the most fearful face, even though they had actually experienced a shock when the middle, less fearful face appeared.
“PTSD patients exhibited greater post-study memory distortion of the fear-conditioned stimulus toward the stimulus expressing the highest fear intensity,” wrote the researchers.
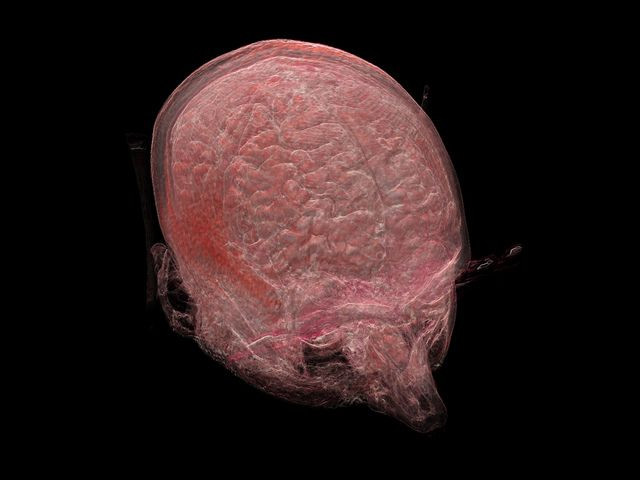
Specifically, the brain areas PTSD patients generalized their trauma to “included areas along the ventral visual stream, such as primary visual cortex and fusiform gyrus, as well as sensory-integration components such as the thalamus, which have strong connections with the amygdala,” noted the authors.
Importantly, the amygdala itself did not show increased activation. This brain region is the seat of our most intense emotions and so naturally acts as a “first responder” to any threat.
The functional brain differences mapped by the researchers provide a model of fear generalization, showing how PTSD symptoms can be triggered by things that merely resemble the original trauma source, say the study authors.
“Current fear conditioning therapies are limited by repeated use of the same cue to trigger the initial trauma,” concluded Morey, who added treatments “might be enhanced by including cues that resemble, but are not identical to, cues in the original trauma.” In other words, more general treatment might go far in treating a more general fear.
Source: Morey RA, Dunsmoor JE, Haswell CC, et al. Fear learning circuitry is biased toward generalization of fear associations in posttraumatic stress disorder. Translational Psychiatry. 2015.
Published by Medicaldaily.com



























