Virus Responsible For Shingles, Varicella Zoster, May Boost Older Adults' Short-Term Stroke Risk
An old childhood foe may return to wreak havoc and increase the risk of stroke in your golden years, suggests a new study published this December in Mayo Clinic Proceedings.
The researchers, studying nearly 25,000 Olmsted County, Minnesota residents over the age of 50, found that those who came down with the viral disease shingles were more likely to suffer a stroke in the three months following their bout than those never infected. Shingles, for the uninitiated, is caused by the same virus responsible for chickenpox, though it only manifests in adults who have previously been infected. This increased risk was present even after accounting for various other factors.
"We found there was a 50 percent increased risk of stroke for three months after shingles, but we also found that people who had shingles had many more risk factors for stroke than those who had not, suggesting they had worse health overall," explained lead author Dr. Barbara P. Yawn, a researcher at the Olmsted Medical Center, in a statement. "The bottom line however is that shingles was still associated with an increased risk of stroke for three months afterwards even when we made allowances for these multiple risk and confounding factors."
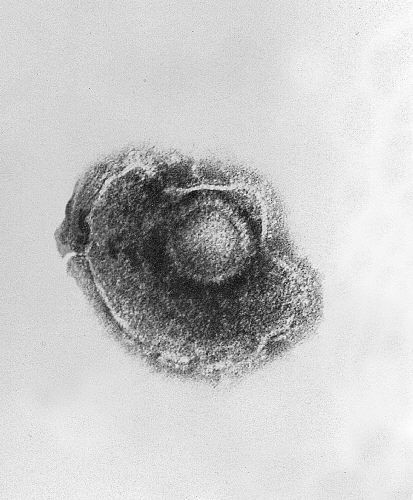
Though shingles, or herpes zoster, can show up in any adult who previously had chickenpox, the virus most often makes its reemergence in people with already compromised immune systems. It does this by remaining dormant in the body, near the spine, after an initial chickenpox infection. Unlike its childhood counterpart, shingles is an excruciating experience, with racking pain and a weeks-long rash. In ten to twenty percent of shingles survivors, this pain endures long after the virus has been beaten back again — a condition known as postherpetic neuralgia (PHN). It’s believed this is due to nerve damage caused by the virus. For a particularly unlucky few, their PHN never goes away.
The link between stroke and shingles has been previously theorized, though not conclusive. In this study, the researchers compared a sample of 4862 residents with a confirmed shingles diagnosis who had lived in the area from 1968 to 2011 with a similarly-matched control group of 19,433 people with no shingles history. Although they did find a temporary boost to stroke risk, their search for an added risk of heart attack between the two groups was unsuccessful, even within the first three months.
Less apparent is how shingles could raise our stroke risk, though Dr. Yawn and her colleagues offered some possible theories. "Recent studies have shown that the zoster virus appears to affect vascular tissues as well as the central nervous system and that it may therefore be a systemic illness," said Yawn. "Another possible explanation is that stroke is a consequence of the inflammatory response that occurs with an acute zoster episode. This increased risk of stroke may be preventable by vaccinating against the zoster virus."
While varcella zoster is found dormant in about 95 percent of adults, and shingles occurs in about one of every three, a vaccine does currently exist and provides a degree of protection against it (around 60 percent). Those vaccinated for chickenpox, provided they never contract the actual disease, are believed to be safe from later developing shingles.
Source: Yawn B, Wollan P, Nagel M, et al. Risk of Stroke and Myocardial Infarction After Herpes Zoster in Older Adults in a US Community Population. Mayo Clinic Proceedings. 2015.
Published by Medicaldaily.com



























