Why COVID-19 Immunity Is So Specific—and Offers Little Protection Against Common Cold Coronaviruses
COVID-19 immunity has often been misunderstood as broadly protective against other coronaviruses, including those that cause the common cold. While SARS-CoV-2 belongs to the same viral family as seasonal coronaviruses, immune protection does not spread evenly across that group. Instead, immune memory formed through infection or vaccination remains sharply focused on COVID-19 itself.
Large immune-profiling studies now show that antibodies and T-cells generated by COVID-19 exposure barely strengthen defenses against long-circulating strains like OC43 or 229E. This explains why people continue catching colds after vaccination and why COVID-19 has settled into circulation without displacing other coronaviruses.
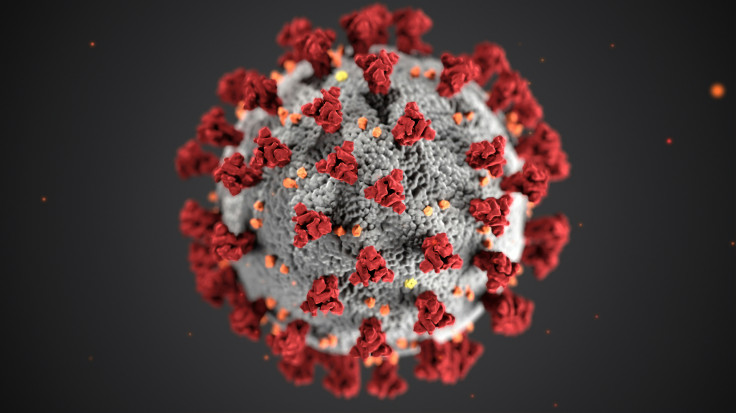
COVID-19 Spike Protein Targeting Explains Immune Specificity
COVID-19 immunity is shaped primarily by how the immune system recognizes viral spike proteins. SARS-CoV-2 spikes consist of two regions: the highly variable S1 domain used for cell entry, and the more conserved S2 domain shared across coronaviruses. Immune responses depend heavily on which region becomes dominant.
Vaccination and infection overwhelmingly train antibodies to bind the SARS-CoV-2–specific S1 domain. This creates powerful neutralization against COVID-19 itself but leaves conserved regions largely untouched. As a result, antibodies struggle to recognize common cold coronaviruses that rely on different spike structures.
Based on a study conducted by researchers publishing in Communications Biology and reported by News-Medical, antibody depletion experiments showed that removing S1-binding antibodies eliminated nearly all SARS-CoV-2 spike recognition, while antibodies against seasonal coronaviruses remained unchanged. This confirmed that COVID-19 immunity forms a narrow, virus-specific profile rather than a broad coronavirus shield.
COVID-19 Immunity in T-Cell and Cytokine Responses
T-cells play a critical role in long-term immunity, particularly when antibodies decline. COVID-19 infection and vaccination both generate strong CD4 and CD8 T-cell responses, but these responses are also highly targeted. Rather than broadly reacting to all coronaviruses, T-cells preferentially recognize SARS-CoV-2 peptides.
Seasonal coronaviruses tend to elicit T-cell responses biased toward conserved S2 regions due to repeated lifetime exposure. In contrast, SARS-CoV-2 drives intense responses across both S1 and S2, creating a separate immune compartment. This separation prevents immune resources from spilling over to common cold strains.
According to the National Institutes of Health, FluoroSpot and cytokine profiling data show that SARS-CoV-2 stimulation produces significantly higher interferon-gamma and interleukin-2 responses than endemic coronavirus stimulation. The NIH also reported distinct CXCL8 inflammatory signaling patterns, reinforcing that COVID-19 immunity operates through a separate immune pathway rather than amplifying existing cold defenses.
Does COVID-19 vaccination protect against common cold coronaviruses?
Marginal antibody rises against OC43/229E unlikely to translate to clinical protection given S1-dominant specificity.
Can prior COVID-19 infection prevent seasonal coronavirus colds?
Minimal cross-reactive T-cells and antibodies suggest no meaningful interference with endemic circulation patterns.
COVID-19 and Endemic Coronaviruses Occupy Separate Immune Niches
Despite global spread, SARS-CoV-2 has not displaced the four seasonal coronaviruses that cause common colds. Serological surveys consistently show near-universal pre-existing antibodies to OC43, NL63, HKU1, and 229E both before and after the pandemic. COVID-19 immunity layers on top of this baseline rather than replacing it.
Hybrid immunity—combining infection and vaccination—produces the strongest SARS-CoV-2 protection yet still fails to meaningfully suppress cold coronavirus circulation. Antibody increases against endemic strains remain small and short-lived, well below neutralization thresholds.
According to the World Health Organization, respiratory virus surveillance confirms that endemic coronaviruses maintained stable circulation throughout COVID-19 waves. WHO analyses indicate that SARS-CoV-2 established its own ecological niche, similar to influenza, without erasing long-standing immunity patterns tied to seasonal viruses.
Why doesn't COVID-19 immunity cross-protect cold viruses?
S1 domain hypervariability drives vaccine specificity bypassing 40-60% S2 homology shared across strains.
How specific is immunity after COVID-19 vaccination?
90%+ antibodies bind SARS-CoV-2 S1 exclusively; depletion removes cross-reactivity confirming narrow targeting.
What This Means for Vaccines and Public Health
COVID-19 vaccines are exceptionally effective at preventing severe disease, hospitalization, and death caused by SARS-CoV-2. However, they were never designed to provide broad protection across all coronaviruses. Expecting fewer colds after vaccination misunderstands how immune targeting works.
These findings support continued vaccine updates focused on emerging COVID-19 variants rather than attempts to rely on spillover immunity. They also explain why cold viruses returned quickly once masking and distancing measures eased. COVID-19 immunity protects where it is aimed—and little beyond that.
Why COVID-19 Immunity Works Exactly as Intended
COVID-19 immunity succeeds by being precise rather than broad. Its strength lies in sharply focused antibody and T-cell responses that neutralize SARS-CoV-2 efficiently without disrupting long-standing immune memory to other viruses. This precision explains both the success of vaccines and the persistence of common colds.
Understanding this specificity helps reset expectations. COVID-19 vaccines are not pan-coronavirus solutions, but they remain one of the most effective targeted immune interventions ever deployed. Clear boundaries between immune responses are not a flaw—they are a feature of a well-trained immune system.
Frequently Asked Questions
1. Does COVID-19 vaccination protect against the common cold?
No, COVID-19 vaccines generate immunity specific to SARS-CoV-2. They do not provide meaningful protection against common cold coronaviruses. Any small antibody increases are temporary and not neutralizing. This is why colds remain common after vaccination.
2. Why doesn't immunity transfer between coronaviruses?
Most immune responses target virus-specific regions like the S1 spike domain. These regions differ significantly between coronaviruses. Conserved regions receive less immune attention after vaccination. This limits cross-protection.
3. Does getting COVID-19 strengthen existing cold immunity?
Only marginally. Studies show small, short-term increases in cold coronavirus antibodies. These increases are not strong enough to prevent infection. Long-term immunity patterns remain unchanged.
4. Will future vaccines provide broader coronavirus protection?
Researchers are exploring vaccines targeting conserved regions like the S2 domain. These approaches aim to widen protection. However, current vaccines are optimized for SARS-CoV-2 control. Broad protection remains experimental.
Published by Medicaldaily.com