Why MERS Isn't SARS, Pt. 3: Most Descriptive Report To Date Cites Major Contrasts Between The Coronavirus Outbreaks
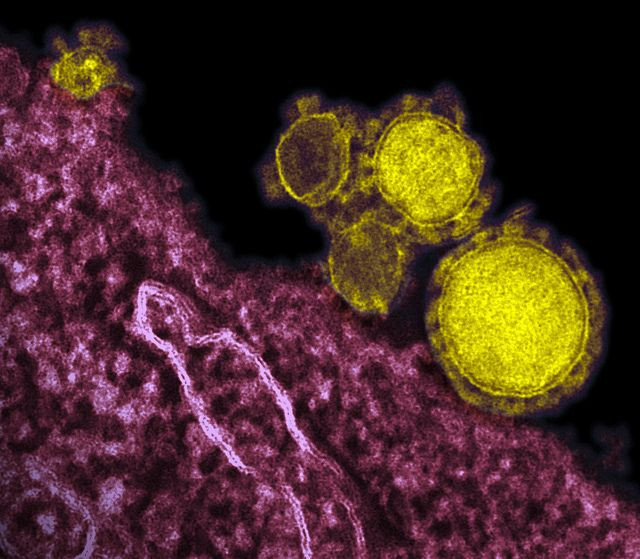
A new report in The Lancet Infectious Diseases outlines some important differences between cases of Middle East respiratory syndrome (MERS) coronavirus and the related SARS virus that plagued the world nearly a decade ago. The description comes from scientists at the Ministry of Health in the Kingdom of Saudi Arabia, where the "lion's share" of MERS cases have been reported.
Last week the World Health Organization opted against designating the MERS outbreak as "an international emergency," and earlier today the global health body announced the risk from the virus towards haj pilgrims was very low.
Despite these developments and studies saying the virus has lacked pandemic potential, experts remain wary that the situation could quickly escalate if the virus mutates. MERS is a close relative of the SARS virus, which killed 774 people throughout 30 countries in 2002-2003
To advance the public understanding of MERS, Saudi health officials reviewed clinical information from 47 of the 90 confirmed MERS infections, making this analysis the largest to date on the disease. These cases comprise two incidences, which occurred between September 2012 to June 2013; one was a hospital outbreak in the eastern city of Al-Hasa, while the other began with an infected man living near the Saudi capital of Riyadh
Overall the data shows that MERS undoubtedly causes a severe respiratory disease that resembles SARS. High rates of cough, fever, and shortness of breath were observed, along with a significant amount of severe intestinal symptoms.
"Despite sharing some clinical similarities with SARS (e.g. fever, cough, incubation period), there are also some important differences, such as the rapid progression to respiratory failure, up to five days earlier than SARS,"* explained Professor Ziad Memish, the Deputy Minister for Public Health from the Kingdom of Saudi Arabia, who led the research.
This "rapid progression to respiratory failure" may explain why MERS has killed a higher percentage of people — 50 percent — relative to SARS, which had 9.6 percent mortality.
But when they looked at who was actually killed by the disease, a major contrasting factor appeared: co-morbidities.
The overwhelming majority of patients who died — 96 percent — had serious pre-existing conditions, such as diabetes, high blood pressure, and chronic heart disease. One out of two fatalities in this group had chronic kidney disease, which is interesting, given higher rates of kidney failure have been observed for MERS relative to SARS.
MERS fatalities have also struck older groups, highlighting the importance of elevated safety measures for this potential at-risk group.
"In contrast to SARS, which was much more infectious, especially in healthcare settings, and affected the healthier and the younger age group, MERS appears to be more deadly with 60 percent of patients with co-existing chronic illnesses dying, compared with the one percent toll of SARS," said Dr. Memish.
"Although this high mortality rate with MERS is probably spurious due to the fact that we are only picking up severe cases and missing a significant number of milder or asymptomatic cases, so far there is little to indicate that MERS will follow a similar path to SARS."
Should we still care about MERS?
Of course!
MERS is still out there, and new revelations about asymptomatic patients suggest the disease may be more widespread than we think.
MERS is a coronavirus — a family of germs that is very widespread. If you've ever had a common cold, then there's a 10 to 15 percent chance that you've had a coronovirus. Learning more about how MERS spreads from person to person — and how to stop it — could teach us valuable lessons that improve public health.
In the study, the authors list about 40 questions about MERS that need answers. Here are some of the most urgent, in their opinion:
What is the origin and the natural reservoir for MERS-CoV?
What is the source of MERS exposure and infection acquired outside health-care facilities: in the household or the community (animals, foodstuff, water, sewage, other)?
Do super-spreaders — people who silently carry/transmit dangerous forms — of MERS exist in the community?
What are the best ways to control and treat MERS?
*How do people catch MERS?
Source: Assiri A, Al-Tawfiq JA, Al-Rabeeah AA et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infectious Diseases. 2013.
Published by Medicaldaily.com



























