Zika Virus May Cause Microcephaly By Crossing Blood-Brain Barrier, Attacking Cells In Cortex
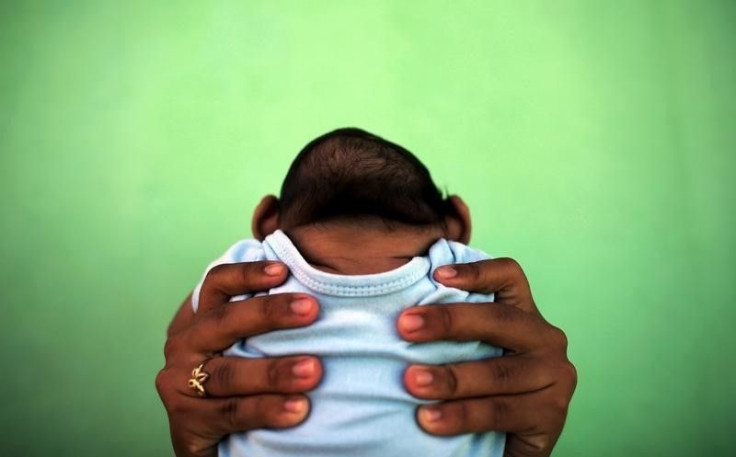
As the Zika virus continues to spread around the world — with 153 travel-associated Zika cases identified in the United States, according to the Centers for Disease Control and Prevention — scientists are scrambling not only to find ways to prevent and treat the disease, but also to understand it. Perhaps the biggest mystery about Zika is how it affects pregnant women and their unborn babies, and whether it causes microcephaly, a birth defect that causes babies to be born with incomplete brains and abnormally small heads. Researchers have been hesitant to conclude that the virus directly causes microcephaly due to a lack of information about the disease's biology.
Now, a new study out of Johns Hopkins University School of Medicine, Florida State University, and Emory University has shed some light on the biology behind Zika, and discovered that the virus specifically infects cells involved in the brain’s outer layer (known as the cortex), preventing them from dividing and growing new brain cells. The researchers examined human stem cells in the lab for their study, and believe the results may lead to new drugs for the disease.
For their experiments, the researchers grew cortical neural progenitor cells — stem cells involved in the development of the brain’s cortex — in the lab, along with induced pluripotent stem cells (capable of growing into any type of cell in the body, including cortex stem cells) and immature neurons. They then exposed all three types of cells to the Zika virus. The researchers analyzed the results, as well as the cells’ genetic expressions during Zika infection.
Ninety percent of the cortical neural progenitor cells were infected within three days of virus exposure. The virus attacked the cells, then used them to produce more viruses. In addition, genes that were used to fight viruses had not been turned on, resulting in most of the infected cells dying. Other genes that maintained cell division and new cell development were also impaired.
“Now that we know cortical neural progenitor cells are the vulnerable cells, they can likely also be used to quickly screen potential new therapies for effectiveness,” said Dr. Hongjun Song, a professor of neurology and neuroscience in the Johns Hopkins Institute for Cell Engineering, in the press release.
Zika virus was first discovered in 1947 in Uganda, but in May 2015 the virus began to spread in Brazil. It’s now considered a public health emergency of international concern (PHEIC) by the WHO. The virus is mainly spread by mosquitos, typically by those that also spread dengue and chikungunya viruses, and there is no vaccine or cure for the disease.
While the latest research may be a big step forward, the researchers note that there’s still many more questions to answer — it will still take more research to formally conclude that the virus causes microcephaly. “This is a first step, and there’s a lot more that needs to be done,” Song said in another press release. “What we show is that the Zika virus infects neuronal cells in dish that are counterparts to those that form the cortex during human brain development.”
Other questions include: Why aren’t adults affected the same way as fetuses? How does the virus cross the blood-brain barrier? And what are other potential neurological defects of the virus in both fetuses and adults? For example, recent research found a link between the Zika virus and a condition of temporary paralysis known as Guillain-Barré Disease, as well as other serious problems, like stillbirth and damaged tissues outside the central nervous system.
“We are trying to fill the knowledge gap between the infection and potential neurological defects,” said Hengli Tang, a virologist studying the Zika, dengue, and hepatitis C virus, in the press release. “The questions we address here are among the very first questions people want to know the answers of.”
Source: Ming G, Song H, Tang H, et al. Cell Stem Cell. 2016.



























