Discovery Of 5 New Breast Cancer Genes Strengthens Case For Personalized Medicine
It’s nice to think that if you regularly slather on high-SPF sunscreen and cut back on the number of burgers you eat you won’t get cancer. While these are certainly healthy habits, each person’s risk for disease depends more on the individual, and the complex genetic changes they accumulate over time — something scientists refer to as the cancer genome.
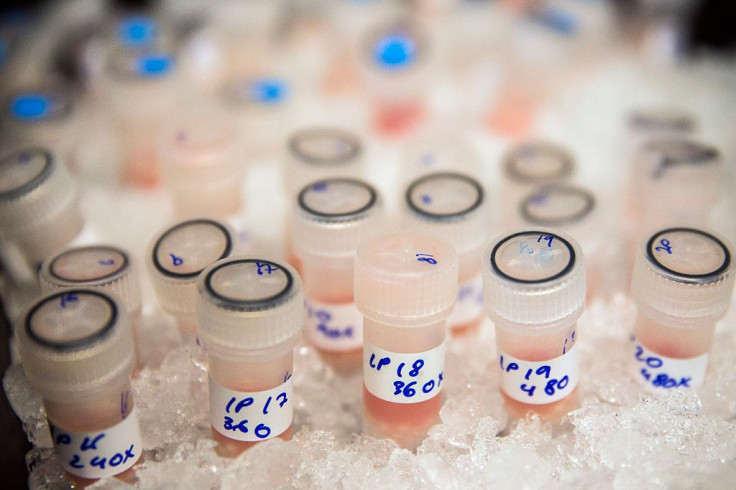
The National Cancer Institute explains that even small changes in a cell can alter the way that cell expresses itself, leading it to grow quickly and possibly damage other cells. That’s why the ability to screen for genetic mutations associated with cancer is a major win. Already, studies have shown that the BRCA1 and BRCA2 gene mutations can increase the risk for breast cancer. Now, a new study published in Nature adds five new genes to look out for.
Curious to pinpoint the exact places these mutations occur in the genes linked to breast cancer, researchers from the Wellcome Trust Sanger Institute and the European Bioinformatics Institute (EBI) analyzed entire breast cancer genomes with computational techniques capable of reviewing each genetic sequence. They found five additional genes associated with the disease, as well as 13 new mutational signatures that influence tumor development. What’s more, these cancer profiles, including those with known mutations, “were highly distinctive from each other and were also very different to other breast cancers,” researchers said.
This is a breakthrough on two levels. First, this is the first study to provide such a large overview of the breast cancer genome, collaborator Dr. Ewan Birney, from EBI, said in a statement. It uncovers new reasons for cancer incidence and provides researchers an unexpected way to characterize breast cancer genes in the future, he added. Second, this data strengthens the case for more precision medicine — a growing trend forecasted to change the way we treat conditions such as obesity.
"In the future, we'd like to be able to profile individual cancer genomes so that we can identify the treatment most likely to be successful for a woman or man diagnosed with breast cancer,” Dr. Serena Nik-Zainal said in a statement.
It seems like a no brainer that doctors would embrace more personalized ways to spot and treat diseases like cancer, but that’s not the case. As Medical Daily previously reported, physicians are still confused about when they should order genetic tests, how to interpret the results, and which of those findings they should share with their patients. In 2007, a study from Arizona State University suggested that personalized medicine raises legal, regulatory, and ethical issues. The liability, though, mostly stems from the lack of training doctors have received in genetic testing.
The push for a more individualized approach to care is meant to improve the fit between patient and treatment, according to the Association for Psychological Science. It would allow for more targeted approaches to medical decision-making, clinical practice, interventions, and — most importantly — treatment. Adopting these ideas would change how doctors treat patients, and change is scary no matter who you are — but at the end of the day, it could be key to driving down cancer rates and ultimately saving lives.
"The intersection of behavior and genetics provides exciting research possibilities," said Dr. Richard Hodes, director of the National Institute of Aging, who was not involved with the Nature study. "If we can determine the extent to which we can tailor behavioral treatments to the unique genetic characteristics of an individual, then we will be on our way to the era of personalized medicine for a variety of conditions."
Source: Nik-Zainal S, et al. Landscape of Somatic Mutations in 560 Breast Cancer Whole-Genome Sequences. Nature. 2016.
Correction: This article orginally incorrectly stated that Dr. Richard Suzman is the director of the National Institute of Aging. The director is Dr. Richard Hodes.
Published by Medicaldaily.com



























