Alzheimer’s Disease: Is There A Cure For This Condition?
The scientific community is abuzz with excitement over a vital clue that might at last lead them to an eventual cure for Alzheimer’s disease.
One of the most significant victories in the frustrating fight to finally cure this incurable disease was made in new study from the laboratory of Harvard researcher Dr. Yakeel Quiroz-Gaviria, PhD. In this study, Dr. Quiroz-Gaviria and her colleagues suggest a new target for drugs that might have the potential to slow down or even stop Alzheimer’s disease in its tracks.
Dr. Quiroz-Gaviria, her longtime colleague Dr. Francisco Lopera and study first author Dr. Joseph Arboleda-Velasquez have developed a viable hypothesis to explain why a single woman in their study was highly resistant to developing Alzheimer’s disease dementia. More interestingly, their work suggests a possible path to a treatment that could be beneficial for all forms of Alzheimer’s disease.
The study published in the November 2019 issue of Nature Medicine is a case report and extensive analysis of this one woman in her 70s. The trio studied a large family in Colombia, South America, whose some family members have a mutation in the presenilin 1 gene that causes early-onset Alzheimer’s disease. Over 1,000 people in this family are affected by the presenilin 1 gene mutation.
Among these family members, early symptoms of Alzheimer’s such as memory loss and word-finding difficulties almost always develop around age 44 then dementia follows at around age 49. The study found some individuals might develop these symptoms or dementia one, two, or even three years later. But, not 10 or 20 years later -- and certainly not 30 years later.
However, there was this one woman in her 70s with this genetic mutation only now starting to show symptoms. The question is, why? The answer led to the invaluable clues that might make future drugs more effective in the fight against Alzheimer's.
Variations in the APOE gene are a risk factor for Alzheimer’s. APOE, the acronym for Apolipoprotein E, is a protein involved in the metabolism of fats in the body. It's implicated in Alzheimer's disease and cardiovascular disease.
APOE has been linked to ordinary, late-onset Alzheimer’s disease. It comes in three common forms. Some 70 percent to 75 percent of people have APOE3. About 15 percent to 20 percent of people have the APOE4 gene, while 5 percent to 10 percent of people have an APOE2 gene.
If a person has one APOE4 gene, his risk of developing Alzheimer’s disease is three to four times more likely than if someone with APOE3 genes. The risk of a person with one APOE2 developing Alzheimer’s disease is somewhat less than the person who has APOE3 genes.
The Harvard team's inquiry into why this single woman with a mutation for early-onset Alzheimer’s had not yet developed dementia found she had an additional mutation in her APOE gene. They found this woman’s mutation of her APOE gene is an unusual variant called APOE3Christchurch (APOE3ch), named after the New Zealand city where it was first discovered.
Even more unusual is she had two versions of this mutation. This means both her father and her mother gave it to her. This finding led researchers to wonder if the APOE3ch mutation could be the cause of her resistance to Alzheimer’s disease.
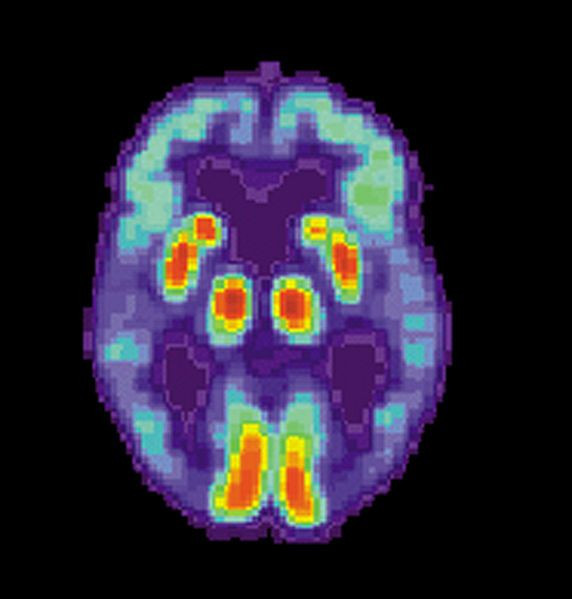
The levels of this woman's tau were also examined. The abnormal protein called tau is associated with the destruction of brain cells in Alzheimer’s disease. Tau is thought to accumulate in the brain after amyloid protein, which is the pathologic hallmark of Alzheimer’s disease, forms plaques.
Although this woman's brain had more abnormal amyloid plaques than most people with full-blown Alzheimer’s dementia, she had relatively little tau. The obvious question now was, could the APOE3ch mutation be related to the small amounts of tau protein?
The answer is far from settled. Researchers, however, did uncover some clues through laboratory experiments. Their findings suggest the APOE3ch mutation might reduce the uptake of tau in brain cells.
In addition, they were able to produce similar beneficial results using a special protein they created in the laboratory in an effort to mimic the effects of the APOE3ch mutation.
Published by Medicaldaily.com



























