Blood Cancer Breakthrough: 94% Of Multiple Myeloma Patients See Remission With New Treatment
A recent clinical trial in China for a new cancer treatment resulted in 94 percent of patients with multiple myeloma going into complete remission. The treatment, called chimeric antigen receptor, or (CAR) T-cell therapy, is a type of immunotherapy procedure that teaches the patient’s own immune system to attack cancerous cells. Though research is still in its early stages and the trial was very small, experts believe this treatment may be our closest shot to finding a cure for MM, as well as other blood cancers.
Of 35 patients with multiple myeloma, 33 saw a complete remission following two months of (CAR) T-cell therapy. Patients did experience side effects, but most were mild and all were temporary. The study was presented at the 2017 American Society of Clinical Oncology (ASCO) Annual Meeting.
"Although recent advances in chemotherapy have prolonged life expectancy in multiple myeloma, this cancer remains incurable," said study author Wanhong Zhao, MD, PhD, in a recent statement. "It appears that with this novel immunotherapy there may be a chance for cure in multiple myeloma, but we will need to follow patients much longer to confirm that."
Read: Blood Cancer Treatment 2017: New Gene Therapy Drug Cured A Third Of Dying Lymphoma Patients
The immunotherapy treatment is customized to fit each patient. First, doctors will collect a patient's T cells. These are white blood cells involved with scanning the body for foreign entities, such as infections, and alerting other immune system cells to find and destroy the intruder. Once harvested, the patient's T-cells are genetically reprogrammed so that they are better able to seek and destroy cancer cells. These reprogrammed cells are them injected back into the patient, with results being seen in as little as 10 days after initial injection.
There are no cases of relapse in patients that have recovered, and all patients who recovered have no detectable cancer cells in their bone marrow.
As far as side effects, Cytokine release syndrome or CRS, a common side effect of CAR-T cell therapy, occurred in 85 percent of patients. In the case of CAR T-cell therapy, the CAR protein is added to the surface of T cells, to better help the T cell find a cancer cell with a matching antigen, sort of like a key fitting into the right lock. When this happens, the T cell destroys the cancer cell. When cells are destroyed, they make cytokines. These are cell-signalling molecules that aid cell-to-cell communication and immune system response. However, in the case of CAR-T cell therapy, sometimes CRS can occur, which is an uncontrolled inflammatory response. When cytokines are released into circulation they can cause a number of symptoms, which vary from mild to life-threatening, such as fever, nausea, chills, hypotension, tachycardia, asthenia, headache, rash, and scratchy throat.
However, CRS in the patients involved in this study was only temporary, and although two patients experienced severe symptoms of the condition, all recovered.
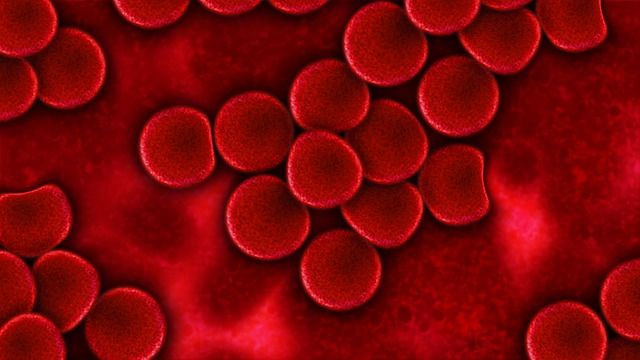
Multiple myeloma is a cancer of plasma cells, and according to the American Cancer Society, is relatively rare, with only about 30,000 estimated cases in the US during 2017. The study results are exciting, but it was extremely small. The researchers plan to test the same treatment on 100 patients at four different hospitals in China and launch a similar study in the U.S. as early as 2018.
See Also:
Common Blood Cancer Drug May Help Treat Severe Asthma, Study Says
Published by Medicaldaily.com



























