Scientists May Make Cancer Immunotherapy Treatments More Precise With Breakthrough Discovery
In a new study published in the journal Science, researchers from Cancer Research UK have identified a new way to sharpen the precision of cancer immunotherapy, a type of treatment that boosts the immune system in fighting and destroying cancer. The research identifies a new method that could help the immune system spot cancer cells based on their complexity and antigens, and then destroy them.
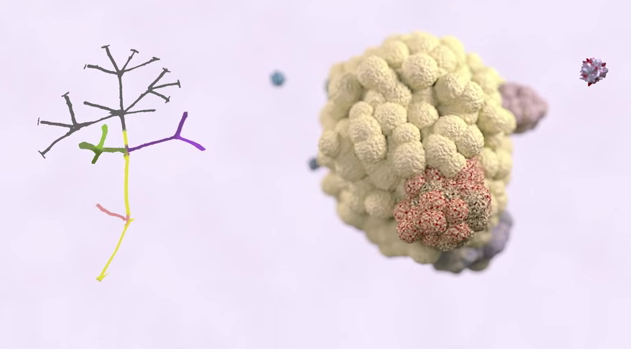
As cancer cells spread, they mutate to avoid the immune system or drugs, and become particularly resilient and difficult to treat. But if scientists could figure out a way to flag cancer cells by their antigens — proteins on the surface of virus-infected or cancer-damaged cells that trigger the immune cells to attack — they would be better equipped to find new ways to boost the immune system. In the future, with detailed information about antigens, researchers might grow immune cells in the lab that can spot these proteins, forming a “fearsome cancer-fighting force, with the potential to target every cancer cell in the body,” Cancer Research UK states in the video below.
“We have been using [a type of software] analysis to predict what sorts of mutations are present across the tumor, so we wondered whether we could also use it to look for antigens shared on all tumor cells,” Dr. Nicholas McGranahan, one of the researchers involved in the study, said in the press release. “We had suspected that the diversity of mutations we see in tumor evolution would be reflected by the antigens present on the cancer cells — but until now we had no proof.”
Immunotherapy is a wide area of cancer treatment and research that has built momentum in recent years. Many different types of immunotherapies have been effective in treating and even potentially curing melanomas, B-cell Chronic lymphocytic leukemia, and non-Hodgkin lymphoma, and are currently being developed to treat nearly every time of cancer, including breast cancer. Recent research showed that 70 percent of multiple myeloma patients recovered with immunotherapy.
There isn’t only one type of immunotherapy; there’s a huge variety of treatments that fall under the umbrella. For example, one common form of immunotherapy is known as immune checkpoint inhibitors, in which drugs inhibit the immune system’s ability to keep itself in check during an immune response. This unleashes a greater immune fury against cancer, whereas the natural immune response wouldn’t be as effective. The first immune checkpoint inhibitor drug to be approved by the FDA is ipilimumab, also known as Yervoy, which is used to treat advanced melanoma. Researchers are also working on developing therapeutic antibodies in the lab which can destroy cancer cells when injected into the body. And there are also cancer vaccines being developed which are made from a patient’s tumor cells and are used to bolster the immune system.
Antigens: The Pieces Of The Puzzle
Ultimately, the researchers discovered that the way antigens were spelled out on tumors could determine which route would be the most effective immunotherapy treatment, as opposed to treating the cancer with a broader stroke. They came to that result through a series of tests and discoveries.
First, the researchers used data from The Cancer Gemone Atlas examining over 200 patients who had one of two different kinds of lung cancer — adenocarcinoma or squamous cell carcinoma. They discovered that patients with adenocarcinoma had far more antigens visible on their tumors, providing the immune system an easier way to attack, and they generally fared better than squamous cell carcinoma patients, whose tumors didn’t show antigens clearly. This proved effective as an antigen prediction method, which would allow immune cells to identify similar antigens on cancer cells.
However, another discovery showed that tumors with plenty of antigens also released an immune-suppressing molecule known as PD-L1, which turned off the immune cells from attacking. This was the tumor cells’ way of defending themselves against the immune system, which would normally identify the antigens and destroy the bad cells.
Finally, one more experiment added another piece of the puzzle. Researchers examined data from a study that had used an immunotherapy drug known as Keytruda that was a checkpoint inhibitor — meaning it stopped immune cells from being turned off by the tumor’s suppressing molecule, PD-L1. They compared the results of the study (how well cancer patients fared after taking Keytruda) to their antigen-prediction program, which could show how their tumors displayed antigens. It turned out that 13 patients had tumors with many shared antigens, and the majority of them (12 patients) improved better than patients who had tumors with a lot of different antigens.
In short, the results showed that there are specific targets for immunotherapy treatments depending on tumor antigen expression. Treatments would need to be honed so that they can be used mainly when tumor cells share many antigens.
“Since the true genetic complexity of a growing tumor began to be revealed a few years ago, we’ve all been scratching our heads trying to work out a way round it,” Professor Charlie Swanton of the Francis Crick Institute, considered an expert in tumor genetics, said in the press release. The work may lead to developing “truly effective treatments for advanced disease that exploit the underlying order in the chaos,” he adds. “It’s incredibly exciting, and although it’s early days, it offers hope that we might just be able to turn the tide against advanced cancer — something we desperately want for our patients.”
Source: Swanton C, McGranahan N, Furness A, Rosenthal R, Ramskov S, Lyngaa R, et al. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science, 2016.
Published by Medicaldaily.com



























