Dangers Of Misusing Antibiotics
Abusing antibiotics might make our bodies more vulnerable to viral infections such as the flu, according to a new medical study about the growing problem of antibiotic resistance.
Antibiotics are only effective against bacterial infections and the discovery they can also weaken our defenses against viruses -- against which antibiotics have no effect -- is a frightening new result from misusing antibiotics.
A new study by researchers from the Francis Crick Institute in London suggests antibiotics could actually "prime" the lungs for viral infections. It shows that gut or stomach bacteria drive a type of protein signaling that helps cells lining the lungs keep the flu virus from spreading.
It seems antibiotic use interferes with this protein signaling and therefore impairs this first line of defense against flu infection.
"We found that antibiotics can wipe out early flu resistance, adding further evidence that they should not be taken or prescribed lightly," said lead researcher Dr. Andreas Wack, Ph.D.
In their study, Dr. Wack and his team used a group of mice with healthy gut bacteria as its baseline. They gave these mice a mix of antibiotics for over four weeks through their drinking water.
The mice were then infected with the flu virus. Researchers also infected some mice they hadn't been treated with the antibiotic mix so they could compare the outcomes.
The team noticed that about 80 percent of the untreated mice with healthy gut bacteria survived the infection with the flu virus. On the other hand, only one-third of the mice that had previously received the antibiotic mix were able to survive the viral infection.
"Inappropriate use (of antibiotics) not only promotes antibiotic resistance and kills helpful gut bacteria, but may also leave us more vulnerable to viruses," noted Dr. Wack.
"This could be relevant not only in humans but also livestock animals, as many farms around the world use antibiotics prophylactically. Further research in these environments is urgently needed to see whether this makes them more susceptible to viral infections.”
Researchers have a theory as to how ingesting antibiotics weakened the mice before their exposure to the flu. They found that type I interferon signaling -- a form of protein signaling regulating the response of a type of cell that lines the lungs -- is key to stopping the flu virus from replicating in the lungs.
Gut bacteria normally drive interferon signaling. It tells the lung cells to react to a virus, stops it from replicating, and makes survival and recovery more likely.
"We were surprised to discover that the cells lining the lung, rather than immune cells, were responsible for early flu resistance induced by microbiota," said Dr. Wack.
Researchers said antibiotic treatment delays the switching-on of an antiviral gene called MxA in humans, which affects the efficiency of the response the body initiates against the virus.
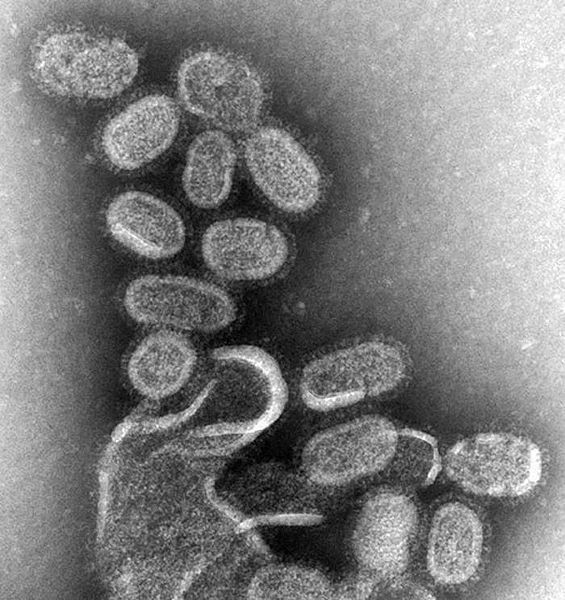
"It takes around two days for immune cells to mount a response, in which time the virus is multiplying in the lung lining," said Dr. Wack.
He said two days after infection, antibiotic-treated mice had five times more virus in their lungs. To combat this deadlier threat, the immune response becomes much stronger and more damaging. This leads to more severe symptoms and worse outcomes.



























