A New Biomaterial Could Be the First Step Toward a Cure for Diabetes
Researchers may have just gotten one step closer to curing Type 1 diabetes, a disease that affects almost 3 million Americans, by creating biomaterials that protect insulin-producing cells during injection. So far, they have successfully injected a diabetic mouse, reversing the symptoms of diabetes in as little as 10 days.
The research was conducted by engineers from Georgia Tech and clinicians from Emory University, and will be published in the June issue of the journal Biomaterials.
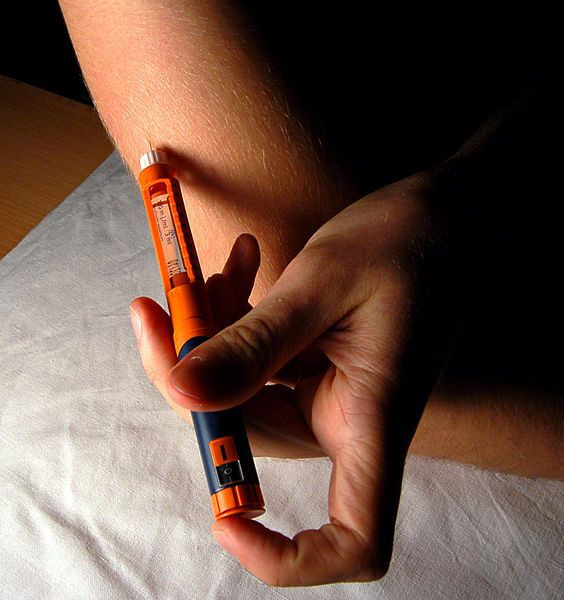
Researchers engineered a hydrogel, which is compatible with biological tissue, to perform two functions during injection. First, it protects a cluster of insulin-producing cells, or donor pancreatic islets, during injection. Once the islets are inside the body, proteins in the hydrogel are able foster blood vessel formation, allowing the cells to successfully graft, survive and function within the body. In this study, the islets were delivered to a site outside of the small intestine - in order to avoid direct injection into the blood stream - where blood vessels were able to grow into the biomaterial and connect with the insulin-producing cells, a news release said.
"It's very promising," Andres Garcia, a professor of mechanical engineering at Georgia Tech, said in the release. "There is a lot of excitement because not only can we get the islets to survive and function, but we can also cure diabetes with fewer islets than normally needed."
Because the researchers were able to use fewer islets than before, they believe it will allow them to treat more patients with limited donor samples - they currently take the donor cells from two to three cadavers to treat one patient.
Four weeks after transplantation, the diabetic mice that were treated had normal glucose levels, and the injected islets were alive and incorporated into the body just as much as islets in a normal mouse's pancreas, however, the study used genetically identical mice, which means that they did not account for immune rejections common in human applications. Coming up with a solution to this problem will be their next step.
"We broke up our strategy into two steps," Garcia said in the release. "We have shown that when delivered in the material we engineered, the islets will survive and graft. Now we must address immune acceptance issues."



























