Debate On Whether Simple Infections Can Lead To Alzheimer’s Intensifies
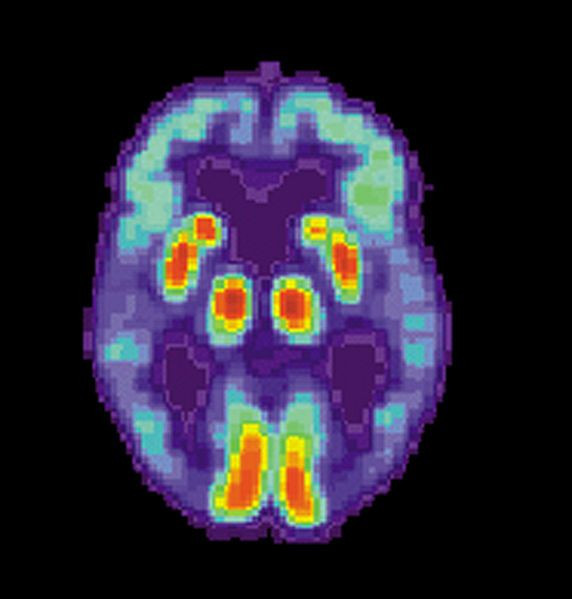
The actual cause of Alzheimer’s disease remains unknown. The current hypothesis proposes that Alzheimer’s is caused by the accumulation of “misfolded proteins” in the brain.
It’s a misfolded protein called amyloid-beta that’s the main component of the amyloid plaques found in the brains of patients with Alzheimer's.
This line of thinking is now changing in favor of a new hypothesis that proposes oral bacteria might be responsible for Alzheimer’s disease. Gaining widespread publicity early in 2019, a new study revealed strong evidence supporting the hypothesis Alzheimer’s might be a result of an infection by the oral bacteria “Porphyromonas gingivalis” (P. gingivalis).
This bacterium produces toxins called gingipains found to accumulate in the brains of patients with Alzheimer's. Gingipains degrade human proteins, giving rise to the deadly misfolded proteins.
Found in the oral cavity, P. gingivalis is implicated in periodontal disease, as well as in the upper gastrointestinal tract, the respiratory tract and the colon.
This finding has led to a rising tide of discussions if there really is an infectious link to Alzheimer's disease
"Ideas in this area of research are still evolving,” said Dr Maria Carillo, PhD, chief science officer of the Alzheimer's Association. “There is now growing evidence that microbes such as bacteria and viruses may play a role in degenerative brain diseases such as Alzheimer's."
Other new research suggests infectious agents could be triggering immune reactions related to plaques and tangles. They suggest the loss of cognitive function in Alzheimer's disease might stem from several different disease processes in the brain, not just one.
A common virus coupled with a genetic factor – namely, the herpes simplex virus 1 (HSV-1) and the APOE4 gene -- can trigger a major risk for Alzheimer's disease, said Dr Ruth Itzhaki, PhD, at the University of Manchester in England.
The accepted viral concept of Alzheimer's proposes HSV-1 in the brain of APOE4 carriers accounts for a high percentage of Alzheimer's cases. It postulates that HSV-1 travels to the brain earlier in life and establishes a latent infection that "leads to viral damage in infected cells and viral-induced inflammation," when activated.
Recent studies have found an increased abundance of human herpesvirus 6A (HHV-6A), HHV-7, HHV-6B, and HSV-1 in post-mortem Alzheimer's disease brains, said Dr Ben Readhead, MBBS, of Arizona State University in Tempe.
"These findings indicate that these species are capable of perturbing host cellular networks that are central to the pathogenesis of Alzheimer's disease and offer testable hypotheses to guide further evaluation of the pathogen hypothesis of Alzheimer's," said Dr Readhead.
The associations seen in laboratory and epidemiological studies, however, do not demonstrate causality, and reverse causation must be considered more likely, said Dr Todd Golde, MD, PhD, of the University of Florida in Gainesville.
He said there's strong evidence an additional hit from an infection can impair cognition, and there's no evidence for causality.
Dr Michael Heneka, MD, PhD, of University Hospital Bonn in Germany said the precise time point in the pathogenesis of Alzheimer's at which bacteria may enter the brain needs to be determined because these phenomena may present just late-stage events.
"Furthermore, it remains elusive how bacteria would overcome the intrinsic innate immune defense of microglia that usually shield the brain from such invasion."
Published by Medicaldaily.com



























