Study finds Novel Way to Prevent Drug-Induced Liver Injury
Researchers have found a novel way to prevent liver damage and improve drug safety by blocking cell-to-cell communication.
Rutgers University and Massachusetts General Hospital researchers said that inhibiting a type of cell-to-cell communication could protect against damage caused by liver-toxic drugs such as acetaminophen.
"Our findings suggest that this therapy could be a clinically viable strategy for treating patients with drug-induced liver injury," said Suraj Patel a postdoctoral researcher in the Center for Engineering in Medicine at MGH and the paper's lead author. "This work also has the potential to change the way drugs are developed and formulated, which could improve drug safety by providing medications with reduced risk of liver toxicity," he said in the journal published in Nature Biotechnology.
The authors noted that drug-induced liver damage is the most common cause of acute liver failure in the U.S. and the most frequent reason for abandoning drugs early in development or withdrawing them from the market. They also said that liver toxicity limits the development of many therapeutic compounds and presents major challenges to both clinical medicine and to the pharmaceutical industry.
While there are no current pharmaceutical strategies to prevent drug-induced liver damage, treatment options are limited.
But researchers have found a new approach that targets the liver’s gap junctions, hollow multimolecular channels that connect neighboring cells and allow direct communication between coupled cells.
Gap junctions in the heart propagate the electrical activity required for synchronized contraction, but their role in the liver has not been well understood, the authors said.
While recent research has shown that gap junctions spread immune signals from injured liver cells to surrounding undamaged cells, amplifying inflammation and injury, their study examined inhibiting the action of liver-specific gap junctions to limit drug-induced liver injury.
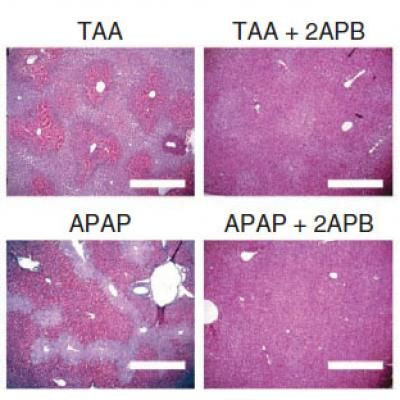
Using genetically mutated mice that lack a particular liver-specific gap junction, the researchers gave them various liver-toxic drugs such as acetaminophen, a commonly used medication best known under the Tylenol brand name.
Acetaminophen overdoses are the most frequent cause of drug-induced liver injury, explained the authors.
The researchers noted that, “compared to normal mice, those lacking liver gap junctions were fully protected against liver damage, inflammation and death caused by administration of liver-toxic drugs.”
The researchers then protected the livers of normal mice against injury and prevented their death by identifying a small-molecule inhibitor of liver gap junctions combined with or even after the toxic drugs.
"This finding is very exciting and potentially very powerful from a number of basic science and clinical application standpoints, which we are continuing to explore," said Martin Yarmush, senior author of the report and the Paul and Mary Monroe Professor of Biomedical Engineering at Rutgers.
"However, before we can think about applying this approach to patients, we need to know more about any off-target effects of gap junction inhibitors and better understand the long-term ramifications of temporarily blocking liver-specific gap junction channels."



























