Breast Cancer Prevention: Why Do Women Facing Higher Risk Turn Down Preventive Therapy?
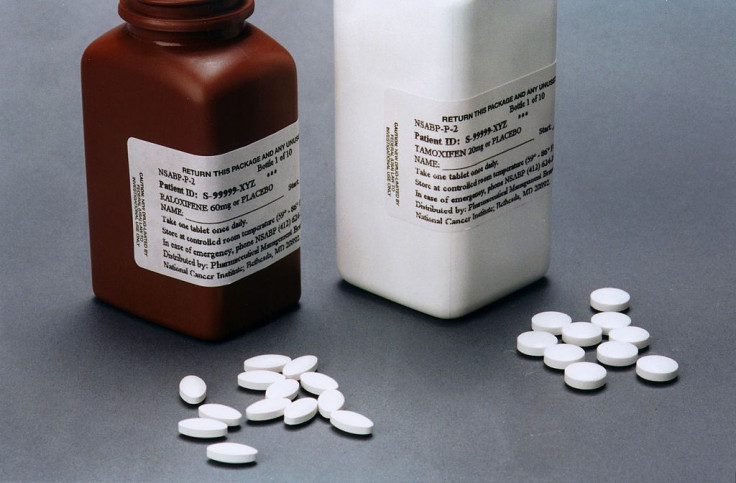
Women who face a higher risk for developing breast cancer have the option of preventive therapy; tamoxifen and raloxifene are both selective estrogen receptor modulators (SERMs) that help reduce women's overall breast cancer incidence and estrogen receptor-positive tumors. However, there has been some concern SERMs result in inadequate levels of uptake and adherence (day-to-day uses of medication). A new study published in the Annals of Oncology aimed to learn more about this, and hopefully finds new data to inform future research and clinical practice.
Study authors hailed from Queen Mary University of London, University College London, Dana-Farber Cancer Institute, and Northwestern University to search for peer-reviewed studies reporting uptake and adherence to this type of preventive therapy; they searched databases, like PubMed, EMBASE, and PsychInfo. Authors described adherence as "either adequate day-to-day use of the medication or persistence with it over time." Each study had to include women aged 18 and older; report quantitative or qualitative data; and use or test SERMs for the purpose of breast cancer prevention. Fifty-seven articles ended up being included for review: 31 reported on uptake and 23 reported on adherence.
Some studies showed clinical factors for greater uptake, such as an abnormal breast biopsy and receiving a physician recommendation. Two studies showed clinically assessed risk was associated with higher uptake, but these results were not consistent. What was, however, was lower uptake in women concerned about contradictions with estrogen.
Overall, study authors wrote, "studies suggested day-to-day adherence to preventive therapy was high, although all data were recorded within two years of initiating therapy." This adherence was particularly high at two-year follow-up, and one study using electronic monitoring systems for monitoring medication adherence (MEMS) also suggested high rates of day-to-day adherence in at least the first six months of therapy.
"A relationship between side-effects and adherence was suggested by reports of lower persistence among women taking tamoxifen compared with placebo and raloxifene," the authors wrote. "However, the quality of side effect assessment was poor."
As for qualitative data, all seven studies were related to women's attitude towards tamoxifen or raloxifene, and their decision to partake in preventive therapy. Five of these reported women who thought themselves to be at higher risk were more likely to use this therapy. The therapy, it seemed, "was considered to be a daily reminder of one's risk, which some women preferred to deny or seek alternative strategies."
Quantitative and qualitative data both showed, in the context of breast cancer prevention, there was low uptake of all SERMs and poor long-term persistence. More worrisome was the fact so many women choose not to take the drugs at all, Dr. Sam Smith said in a press release. With a cumulative sample of over 21,000 women, only one in six decided to take preventive therapy. Smith, from Queen Mary University, said if women do take them, they stop taking them before completing the course.
"We need to find out more about how women at higher risk of breast cancer make decisions about the different ways they can reduce the risk of developing the disease, to make sure that they have the information they need to make the choice that is right for them," said Martin Ledwick, Cancer Research UK's head cancer information nurse.
Data from this analysis may not be enough to change current clinician recommendations, but it may make the case for discussing the risk and benefits of preventive therapy with women in order to better inform their decision.
Source: Smith SG et al. Factors affecting uptake and adherence to breast cancer chemoprevention: A systematic review and meta-analysis. Annals of Oncology. 2015.
Published by Medicaldaily.com



























