Federal Regulators to Decide the Fate of Experimental Drugs Linked to Bone Decay, Joint Failure
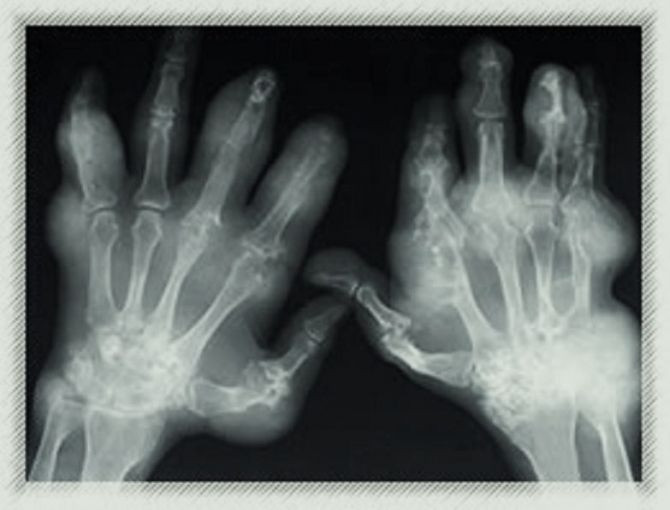
Federal regulators have asked an advisory panel whether human trials on a class of experimental pain medications designed to treat osteoarthritis and chronic back pain should resume after it was temporarily halted in 2010 after the drugs were reportedly causing bone decay and joint deterioration.
Pfizer Inc. and Johnson & Johnson, the two biggest U.S. makers of health-care products, and Regeneron Pharmaceuticals are expected next Monday, March 12, to argue for resuming the clinical trials on the drugs after taking necessary safety precautions to protect their patients.
The U.S. Food and Drug Administration said that the development of this class of anti-nerve growth factor pain drugs “represent a potentially significant and novel strategy” for treating a variety of chronic painful conditions including osteoarthritis, chronic low back pain, diabetic peripheral neuropathy, post-herpetic neuralgia, chronic pancreatitis, chronic prostatitis, endometriosis, interstitial cystitis, vertebral fracture, thermal injury, and cancer pain, according to a memo posted on the FDA website on Thursday.
However, the health agency said that it had to put almost all clinical trials of the drugs on hold in 2010 after an “unusually high incidence in the populations studied” reported joint-related destruction or side effects that were “usually severe” compared to joint-related problems that occur in the patient population, according to the memo. About 500 participants had to have their joints replaced after taking the experimental pain medication.
The only people who companies were still allowed to keep on clinical trials were patients with terminal cancer and had severe pain in their bodies because the benefits in this population were judged to outweigh the risks.
FDA’s outside advisers will consider and vote on whether the three drug maker will be allowed and how to safely resume clinical trials on the injectable nerve-blocking drug, which analysts had once predicted would generate as much as $11 billion a year, according to Bloomberg.
The panel could recommend that certain conditions must be met to resume testing like limiting the drug to lower doses or limiting the participants to only those with fewer existing treatment options.
Previously the drugs have been experimented on people with common conditions like low back pain and osteoarthritis, or damage to the joints caused by aging, a condition that affects about 27 million adults in the U.S. and can cause chronic disability. However, the drugs have also been tested on smaller populations like people with bladder pain syndrome.
The drugs block a protein called nerve growth factor (NGF), which plays a part in promoting the survival and development of sensory and sympathetic neurons, and may also help repair wounds and the growth of new blood vessels, the FDA said.
The joint problems associated with the drug may be that it blocks the beneficial growth effects of the NGF protein, an FDA reviewer said.
“Having a public discussion of this topic at an advisory committee meeting is unusual in that these products are still in the investigational new drug phase of development and are not already approved or under review as new drug applications,” Bob Rappaport, director of FDA’s division of anesthesia, analgesia and addiction products, had written in the staff report.
"Considering what is known thus far about the risks and benefit associated with this class of biologic agents, are there any populations for which further clinical development would be acceptable?" asks one agency discussion question in the Thursday memo.
Doctors have treated pain with common drugs like aspirin and Advil, or powerful opiate-based drugs for more than a century. However both of these current pain medications carry health risks. Anti-inflammatory painkillers like Advil can cause internal and stomach bleeding, while opiates are highly addictive.
The drug makers are expected to argue that patient joint deterioration was most likely caused by the drug’s rare side effect when patients are on multiple painkillers at the simultaneously. Pfizer and J&J found that the bone problems happened mostly in participants taking the experimental drugs along with traditional anti-inflammatory painkillers, according to briefing materials.
Pfizer had also noted that joint problems had been reported with anti-inflammatory drugs since the 1960s, even though the exact cause of the anti-inflammatory drugs link to osteoarthritis had never been established. The drug maker also suspects that some patients who experienced joint problems may have been predisposed to bone fractures that intensify arthritis.
The health agency’s Thursday memo supports the companies’ theory that the side effects were worst among patients taking both the new drugs and older painkillers, but FDA noted that Pfizer's tanezumab was still linked to bone problems when used alone.
Published by Medicaldaily.com



























