Genetic Screening And Sequencing Reports Do Not Inspire People To Change Bad Habits
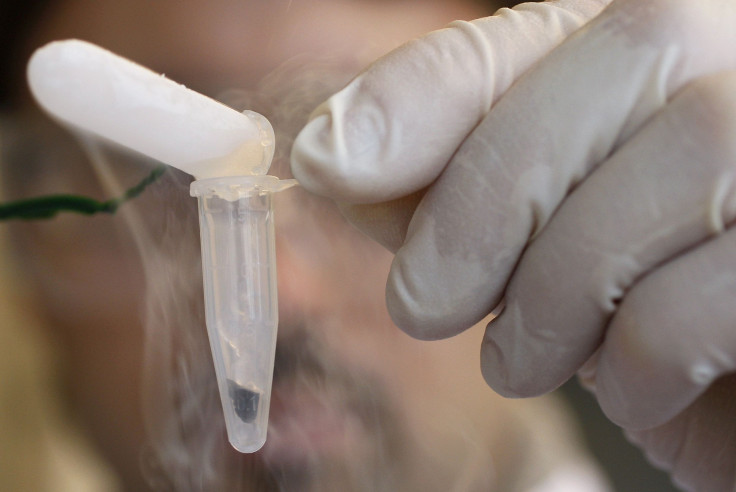
Genome sequencing reports that decipher each and every adenine, thymine, guanine, and ccytosine encoded within your DNA can tell you whether or not you carry genetic mutations that increase your risk of various diseases. Such services beg the question, if you knew you were at risk for a disease, would you change how you live?
Most likely not, say University of Cambridge researchers. Their new study suggests genetic tests that estimate your risk of developing diseases, such as heart disease or certain cancers, do not motivate people to adopt healthier behaviors. The team also explored whether negative findings might demotivate people and spin their behavior in the opposite direction, yet the genetic reports failed in this regard as well. All told, a genetic test showed little demonstrable impact on behavior.
“At best, it has only a small effect on risk-reducing behavior,” concluded the researchers, led by Dr. Theresa Marteau, director of Cambridge’s Behavior and Health Research Unit.
Market Forces
Health care practices increasingly use genetic testing for diagnostic and treatment purposes. Slightly more than a decade ago, products investigating a range of common diseases first became available for consumers, wrote Marteau and her colleagues in their introduction.
“The tests continue to be sold in Canada, the United Kingdom, and other European countries, including Denmark, Finland, the Netherlands, Sweden, and Ireland, with continued international expansion likely,” the authors wrote.
In the United States, the Food and Drug Administration initially limited commercial sales of genetic testing kits. However, some commercial companies, including 23andMe and Pathway Genomics, recently resumed or began sales of health-related services.
Accuracy of test results was and is the regulatory agency’s concern, as one FDA warning letter indicates.
“If the BRCA-related risk assessment for breast or ovarian cancer reports a false positive, it could lead a patient to undergo prophylactic surgery, chemoprevention, intensive screening, or other morbidity-inducing actions, while a false negative could result in a failure to recognize an actual risk that may exist,” wrote Alberto Gutierrez, an FDA director.
Consumer test kits remain controversial for other reasons as well. Knowing you carry a genetic variant does not mean you will necessarily develop a disease. After all, no one gene is the cause of certain complex diseases, including diabetes and some cancers, which require interaction of dozens — possibly hundreds — of genes combined with behavior and environmental factors. Still some people contend commercial tests empower consumers to take charge of their health and tweak their behavior in line with the results.
To understand if this argument holds water, the Cambridge researchers analyzed 18 studies, all of which looked at whether genetic testing for common complex diseases influenced people’s health-related behavior.
Communicating Risk
“The 18 studies included in our review presented the results in a variety of ways,” Marteau told Medical Daily in an email. “Often people were presented with a numerical estimate of the lifetime chances of developing a disease such as diabetes. They were also told which behaviors they could change that could reduce these chances.”
For instance, the report for someone with a high risk of developing diabetes would advise physical activity, in line with government guidelines, and healthy weight maintenance.
Analyzing the studies, the researchers discovered no evidence that people changed their behavior to avert risk of a disease. They also found no evidence to support concerns that information might demotivate or discourage people from changing their behavior, either.
Marteau offers two possible explanations for these results.
“The risk concerns longer term threats, [such as the possibility of developing diabetes in the next 10 years], rather than immediate threats, [such as the possibility of death from swimming in crocodile infested waters],” she said. The latter condition is simply more likely to inspire personal change. She ventured one other possible reason for the apparent lack of action based on her own and other studies.
“The behavior to be changed is one that is routine or habitual, [such as eating cookies with coffee],” she said, and such habits may be made especially easy due to a surrounding environment “with a ready supply of tasty, cheap cookies and coffee.”
Ultimately, this review does not provide the necessary evidence in support of using genetic testing as part of health policies to change behavior to prevent common complex diseases. Marteau, though, does not write off the tests completely. Supplemented by an offer of successful behavior change interventions, they might provide some benefit even if “DNA risk information may not be a necessary pre-condition for their effectiveness,” she said.
More to the point, the tests could be used to categorize people into risk groups, where screening, medication, or surgery might be offered to those at highest risk as a way to prevent poor health.
Source: Hollands GJ, French DP, Griffin SJ, et al. The impact of communication genetic risks of disease on risk-reducing health behavior: systematic review with meta-analysis. BMJ. 2016.
Published by Medicaldaily.com



























