New Breast Cancer Blood Test Screens For Risk Of Non-Hereditary Forms Of The Disease
A new blood test is in development to screen for breast cancer risk among women who don’t carry a BRCA1 gene mutation. While the mutation occurs in roughly 10 percent of breast cancer cases, allowing scientists to understand its role, that still leaves 90 percent of breast cancers unexplained.
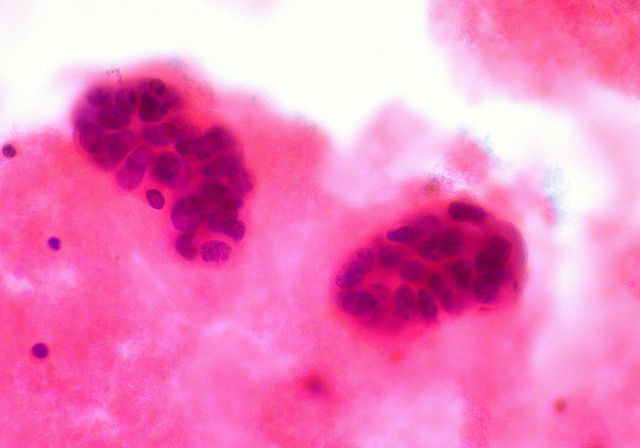
The new research comes from University College London (UCL), where scientists are testing the epigenetics of women without BRCA1 but who still show the same high-risk signs. More basically, they’re looking for certain genetic switches — genes that are switched either “on” or “off” — to determine how women with breast cancer, but no gene mutation, show their DNA in cells. In epigenetics, the field of study related to how genes are activated, this is known as a “signature” — the specific way DNA is reflected through gene activity.
In the latest study, the team looked at blood samples from two large cohorts of women, several years before their breast cancer developed. Some women had BRCA1 mutations; others didn’t. When the team compared the epigenetic signatures from each group’s blood, they found those women who had non-hereditary cancers all carried the same signature. This finding surprised the researchers, as the signature “was able to predict breast cancer risk several years before diagnosis,” said Professor Martin Widschwendter, the study's lead author and Head of UCL’s Department of Women's Cancer, in a statement.
Breast cancer is the most common cause of cancer among women, regardless of race or ethnicity, according to the Centers for Disease Control and Prevention. In 2010, the last year the data was available, nearly 207,000 women and just over 2,000 men were diagnosed with breast cancer. While mammograms are decidedly the go-to method for cancer detection, recent research suggests they aren’t nearly as effective as their reputation leads on. This has led to scientists exploring alternate detection routes, such as 3D mammography, and prevention efforts before cancer starts.
Often, these preventative efforts rely on blood tests, which themselves rely on biomarkers to inform physicians about a person’s health. Biomarkers are essentially substances found in the body, such as protein or enzyme levels, that indicate the presence of a larger disease. Typically, cancers that are hard to detect rely on these smoke signal-type diagnoses. Prostate cancer is a good example. Nestled deep within a man’s body, the prostate gland doesn’t naturally lend itself to immediate observation. For late-stage diagnoses, doctors rely on protein-specific antigen (PSA) tests to see what’s going on.
Much of the same principles are under way with UCL’s latest research. If the team can refine the blood test, to find out for instance whether the test reveals the risk of cancer or its progression in the body, too, it may find a home in clinical settings. "The data is encouraging,” Widschwendter said, “since it shows the potential of a blood based epigenetic test to identify breast cancer risk in women without known predisposing genetic mutations."
Source: Widschwendter, et al. Genome Medicine. 2014.
Published by Medicaldaily.com



























